World-class stroke and heart care in Chester County

Paoli Hospital prepares to open state-of-the-art interventional labs
In the coming months, Paoli Hospital, part of Main Line Health, will welcome new, state-of-the-art interventional labs, offering the most advanced diagnostics and treatment available for patients experiencing stroke and heart disease.
The meticulously designed space will include five dedicated, state-of-the-art labs for neurointerventional, cardiac catheterization and electrophysiology procedures and 11 private, well-appointed patient areas for pre- and post-procedure care. Features include the most advanced imaging equipment available to guide interventional procedures, unparalleled amenities to ensure patient comfort and a collaborative environment where a highly trained team of experts can interact with ease.
Once the new Interventional Labs open, Paoli Hospital will have the capabilities to perform a myriad of complex procedures currently available at other Main Line Health institutions, namely the comprehensive neurointerventional offerings at Bryn Mawr Hospital, and in the near future, more sophisticated structural heart procedures.
We sat down with four of the physicians who will be caring for patients in the new suite ― vascular neurologist, neurointerventionalist and site director of neurointervention for Paoli Hospital Sumeet Multani, MD; vascular and general neurosurgeon and neurointerventionalist Thana Theofanis, MD; electrophysiologist Matthew Goldstein, MD; and interventional cardiologist Aaron Giltner, MD ― to learn more about what the new labs will offer, what makes them exceptional and how this will impact patient care.
Let's begin with the two neurointerventional labs that will be part of the suite. Can you define this term?
Dr. Theofanis: Neurointervention ― or endovascular neurosurgery ― is the use of advanced imaging and 3D technology to diagnose and treat various diseases and conditions in the brain. We're able to pass tools through a patient's blood vessels using a catheter ― a small, thin tube ― preventing the need for patients to undergo open brain surgery.
What does this mean for the Chester County community?

First and foremost, it means patients in need of time-sensitive treatment for stroke will be able to receive care right here at Paoli Hospital. This is critical for patients suffering from ischemic stroke, meaning there is a major blockage ― or clot ― in a blood vessel in the brain, requiring immediate attention. That's when every minute counts.
Dr. Multani: In stroke care, many people have heard the expression, "time is brain." Every minute we lose before administering treatment for stroke, the patient is losing millions of neurons ― or brain cells. And what is lost cannot be recovered.
Stroke is the leading cause of disability in the U.S., and timely treatment is the difference maker. Now, we'll be able to provide lifesaving and lifechanging stroke treatment within minutes of diagnosis. Without this capability, we have to transfer patients to a thrombectomy-capable institution like Bryn Mawr Hospital, losing precious time. Offering these services at Paoli Hospital will have an enormous impact on patient outcomes.
What will make it possible to provide this advanced care at Paoli Hospital?
Dr. Multani: There are two critical components ― the subspecialty-trained clinical team and the physical infrastructure. Our team of experts includes neurologists; neurosurgeons; neuroradiologists; emergency room physicians who can quickly identify stroke and move patients to the interventional suite; cardiologists; nurses; advanced practice providers such as physician assistants and nurse practitioners; rehabilitation specialists and physicians who manage patient care on a long-term basis.
Dr. Theofanis and I, who are part of the neurointerventional team at Bryn Mawr Hospital, will be spending the majority of our time at Paoli Hospital.
Dr. Theofanis: Regarding the clinical team, it's important to note the partnership between Main Line Health and Jefferson Neurosurgery. Our physicians, including myself and Dr. Multani, are also part of Jefferson. I received my training there and continue to collaborate closely with our colleagues at Jefferson Hospital on a daily basis. This means our patients at Paoli Hospital have direct access to the world-class neurosurgical care Jefferson is known for, including access to the latest clinical trials.
Dr. Multani: What also makes this possible is the physical infrastructure. We are building brand new labs from the ground up, equipped with the most advanced imaging capabilities available. The complex procedures we perform require guided imaging that can only be provided by state-of-the-art imaging equipment.
Our labs will feature biplane imaging, which means we can access two views at once, allowing us to view the blood vessels in the brain from the front and the side simultaneously. This allows us to capture the incredibly detailed views we need to guide our interventional procedures.
What procedures will be performed in the new labs?
Dr. Theofanis: We can treat both types of stroke ― ischemic, which is a major blockage in the brain, and hemorrhagic, which refers to any type of bleeding in the brain, such as a ruptured aneurysm.
We'll also treat malformations in the brain and conditions such as subdural hematomas. We use several different approaches depending upon individual circumstances. With stroke, we're able to insert tiny catheters through the groin or wrist to deliver clot-dissolving medicine or to physically retrieve a clot. We may use endovascular coiling to address an aneurysm or a malformation, which involves going through the catheter to insert a platinum coil that serves as a plug to block further blood flow.
We can perform an embolization, which involves applying glue to shut down the blood supply to a hematoma. And we can use carotid stents in the neck to open up a blockage or prevent a future blockage.
What is Viz.ai and how does it impact patient care?
Dr. Multani: Viz.ai is the technology used by the Main Line Health neurointerventional team to ensure patients experiencing stroke get the best and fastest care possible. We have software connected to our scanning equipment that uses artificial intelligence to detect a clot and then immediately alert the entire multidisciplinary team on our cell phones.
Where it previously took 20 to 30 minutes for a scan to be read by a radiologist and the team to be notified when a clot is detected, we can now mobilize in minutes. And we're able to view all the images immediately through the app on our phones or computers, and communicate directly with our colleagues regarding next steps.
What else should patients know about the neurointerventional program coming to Paoli Hospital?
Dr. Theofanis: What we provide is so much more than "treating a picture." We critically evaluate every patient, consider the available options and make the best recommendations for that individual. If an endovascular approach is not appropriate, we have the capability to perform open surgery as well. My partners and I work collaboratively to provide the best outcome for every patient.
Furthermore, we're doing so much more than building neurointerventional procedural labs. We're bringing our entire comprehensive program to Chester County ― the complete continuum of care. This includes aftercare, rehabilitation at our own Bryn Mawr Rehabilitation Hospital and the long-term management of patients by highly skilled physicians. This is an absolute game-changer for the community.
Let's shift our focus from neurointervention to the new cardiovascular interventional labs. Can we begin with a definition of this term?
Dr. Goldstein: Interventional cardiology involves the use of nonsurgical techniques to diagnose and treat coronary artery disease, vascular disease, structural heart disease and congenital heart defects. The field of cardiology is evolving rapidly, and many procedures that traditionally required open heart surgery can now be managed with an interventional approach.
Dr. Giltner: Our team of highly trained subspecialists uses interventional approaches to address numerous conditions, including aortic valve stenosis, mitral valve regurgitation, aortic aneurysm, atrial defects, heart arrhythmias and more. We're able to open blockages, repair holes and damaged valves, and insert special devices to help the heart function properly.
What do the new Paoli Hospital Interventional Labs mean for heart care in this area?
Dr. Giltner: While we already perform a number of advanced cardiovascular interventional procedures at Paoli Hospital, the state-of-the-art equipment in our new labs and the expanded space will allow us to perform even more complex procedures as well as serve a greater number of patients. The most significant addition will be the ability to perform structural heart procedures.
Dr. Goldstein: The physical configuration of the new suite is the key. The five interventional labs ― three of which are dedicated to cardiovascular procedures ― are in one combined unit, leading to significantly greater collaboration among the many different clinical teams.
The best cardiovascular care requires a multidisciplinary approach. Now, when we need another set of hands, or an expert from a different specialty, that person is only a few feet away. It facilitates immediate interaction and the continuous sharing of best practices. This proximity will make each of us better and enhance the care we provide to our patients.
What capabilities will the new interventional labs offer to heart patients?
Dr. Giltner: Two cardiovascular labs will be primarily dedicated to cardiac catheterization procedures, which involve the insertion of a small, thin tube through the wrist or leg into the heart to treat damaged, weakened or blocked vessels. This allows us to place stents and perform balloon angioplasties.
A third lab will be primarily dedicated to electrophysiology procedures, which involve diagnosing and treating electrical concerns, such as arrhythmias.
A fourth "flex lab" will be able to accommodate cardiovascular and neurointerventional procedures. This is where our physicians can, as a team, perform advanced structural heart procedures, such as a cutting-edge treatment known as Watchman, which Dr. Goldstein currently performs at Lankenau and will soon offer at Paoli.
Dr. Goldstein: Watchman is a breakthrough treatment for patients with non-valvular atrial fibrillation who are at risk for stroke but don't tolerate traditional blood thinners.
The Watchman device is implanted in the patient's left atrial appendage (LAA) to close off that section, which prevents harmful blood clots from forming and entering the bloodstream, leading to a stroke. It's an outstanding alternative to taking blood-thinning medications long term, which can present its own set of risks and challenges. This represents the most innovative kind of structural heart work, which soon will be available in our own backyard.
What equipment is required to make all of this possible?
Dr. Goldstein: Cardiovascular interventions require the use of image guidance. We'll have the highest quality imaging equipment available with the lowest levels of radiation. In fact, many of our electrophysiology procedures now require no radiation at all.
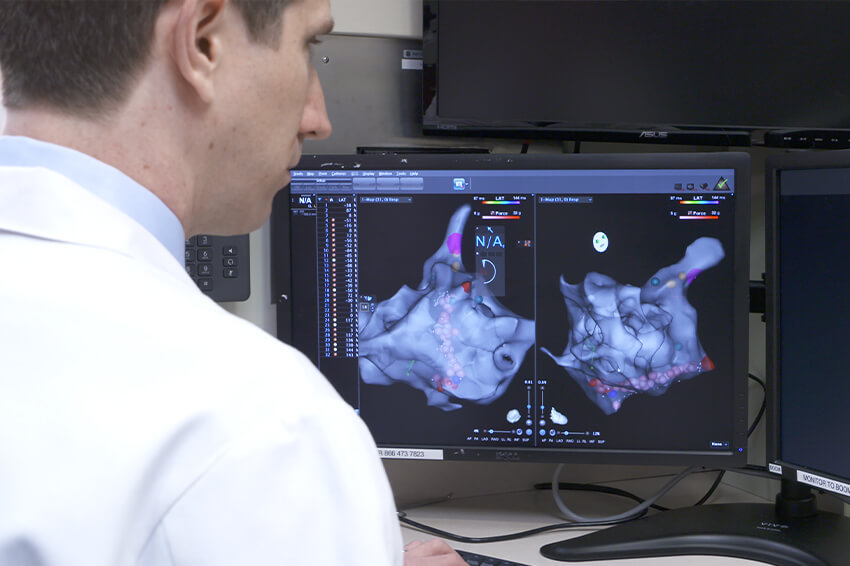
We'll utilize the combination of a state-of-the-art 3D mapping system to map the heart's electricity from the inside, along with traditional ultrasound and ultrasound inside the heart, to get the most detailed and individualized view of the patient's anatomy possible. We call this multi-modality imaging. It allows us to precisely pinpoint where we're going and zero in on the source of the problem.
Dr. Giltner: Every individual's anatomy, blood vessels and heart are completely unique and structurally different. When we use the most powerful imaging available to produce pictures with outstanding quality, our procedures are safer, faster and much more individualized. And this equates to the best results for our patients.
How will the new Paoli Hospital Interventional Procedural Labs impact patient care in Chester County?

Dr. Giltner: We're enormously proud that Paoli Hospital ― and all four of Main Line Health's acute care hospitals ― are recipients of the 2021 American Heart Association (AHA) Mission: Lifeline Award, recognizing quality improvement measures that ensure cardiovascular patients receive efficient and coordinated care, ultimately leading to more lives saved, shorter recovery times and fewer returns to the hospital. The capabilities we're adding through our new interventional vascular suite will make Paoli Hospital an even more outstanding destination for cardiac care.
The Paoli Hospital Interventional Procedural Suite will provide world-class care to the surrounding community and is expected to open late this year.
Next steps:
Learn about the program or donate today
Learn about stroke care at Main Line Health
Learn about heart disease care at Main Line Health
 Content you want, delivered to your inbox
Content you want, delivered to your inbox
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
